
We are now two and a half years into the COVID pandemic, and just beginning to see yet another case surge with the arrival of the BA.5 Omicron sub-variant. The good news just keeps coming! 😉
Along with new variants, 30 months has also given us a lot of research and data. Metajournal alone has indexed almost 39,000 COVID-related publications relevant to anaesthesia, pain, critical care and emergency medicine.
Of course that's a crazy volume of research to manage, with a pretty low signal-to-noise ratio. Sifting through that for quality and relevant studies is exactly what metajournal was designed for.
Here's a quick round-up of interesting COVID-related research...
RAT tests & infectiousness
As good quality, locally validated RAT tests become increasingly available, we are also collecting more data showing they are a good indicator of individual infectiousness at the moment in time the test is performed.
The article collection 'Does a COVID RAT-negative result mean non-infectious?' explores several of these studies, suggesting that a negative RAT is likely a reliable indicator of being non-infectious.
The bottom line...
A correctly-performed adequately-validated RAT, is likely a sensitive indictor of individual infectiousness at that specific moment in time. The reliability of a negative RAT will be improved if using the same manufacturer and technique as a previously positive test, and more so if there are several subsequent negative RATs.
Return to exercise after COVID?
A recent J Sci Med Sport editorial (Hughes 2022) from Australian elite sport, exercise medicine and sports cardiology experts, provides reassuring encouragement when returning to exercise after COVID recovery.
The authors first note that:
"...with over 6 million cases recorded in Australia & NZ in the first 4 months of 2022, and few reports of serious adverse outcomes with exercise, the approach to return to exercise has become more pragmatic."
The authors' experience has been that most vaccinated elite athletes achieve pre-morbid fitness levels by day 7-14 post COVID recovery. Recreational athletes are recommended to pursue a more conservative course, but nonetheless they suggest:
"...a quick return to moderate exercise with a more cautious return to higher intensity exercise."
For those with no or minimal symptoms, the authors describe a graduated approach of exercise return over 6 days (days 1-3, 50% intensity for 15-30 min, then days 4-6, 75% intensity for 30 min), culminating in return to normal activity on day 7, if the graduation is well tolerated.
Interestingly these guidelines are very similar to Jewson's 2020 roadmap for return to activity after COVID infection, developed by the Australasian College of Sport and Exercise Physicians.
Jewson (2020) described three risk categories:
- Low: Under 50 years with mild illness resolving within 7 days.
- Intermediate: prolonged symptoms (>7d); persistent SOB or chest pain; pre-existing comorbidities; elite/endurance athletes.
- High: hospitalised with COVID; SOB or chest pain at rest; cardiac abnormalities.
Jewson's graduated return to physical activity:
- Begin after 10 days of rest and when 7 days symptom-free.
- Begin with 15 minutes of light activity, with gradual increase guided by lack of fatigue with activity.
- 🚩 Red flag symptoms: chest pain, palpitations, severe dyspnoea. STOP & medical review.
Key takeaway
For those with mild or asymptomatic COVID infections, a careful graduated return to exercise can begin soon after recovery from COVID, while monitoring for excessive fatigue and cardiorespiratory symptoms.
Which N95/P2 respirators most often pass Fit Tests?
Ng and co. out of Australia's Royal Melbourne Hospital published excellent audit data answering this very question after Fit Testing 2,161 healthcare workers.
Why is this important?
Many healthcare workers and significantly, the general public, may not have access to formal Fit Testing. We also know that as face shape varies among individuals, so does the effectiveness of protection for different mask types – this is particularly significant for women who have more difficulty in finding suitably-fitting N95 respirators. (Notably 73% of Fit Tested staff in this study were women.)
The results of this study may allow individuals to make educated choices on suitable masks even when they do not have access to Fit Testing, as well as guiding institutional mask purchases.
What did they find?
Three-panel flat-fold N95 masks performed best (3M Aura 9320A+) both for fit test (96% pass) and wearer comfort and usability.
The other three tested designs were not as performant:
- Semi-rigid cup type (3M 1860 or 1860S): 65% FT pass.
- Duckbill type: (BSN ProShield or Halyard Fluidshield): 59% FT pass.
- Flat-fold cup type: (BYD Care DE2322): 32% FT pass.
Final word?
Three-panel flat-fold N95 masks performed best for both fit test (96% pass) and wearer comfort and usability.
Novavax vs Omicron
Nuvaxoid (NVX-CoV2373), the protein-subunit COVID vaccine developed by Novavax, was already shown to be safe and 90% effective against the Alpha (B.1.1.7) SARS-CoV-2 variant – but now we have early release data showing similar efficacy against Omicron and it's various sub-variants (including the surging BA.5).

"...the data indicates a booster shot of Novavax’s vaccine generates neutralizing antibody responses to Omicron variants comparable to what was seen against the original strain of SARS-CoV-2 at the peak of its initial Phase 3 trial."
It is thought that Nuvaxoid's protein subunit structure provides much broader cross-neutralising antibodies than mRNA vaccines, such as from Moderna and Pfizer.
Interesting, animal studies show that the original Nuvaxoid vaccine results in similar neutralising titres to BA.5 as does a new, Omicron BA.1-specific formulation.
Bottom-line...
The current Nuvaxoid vaccine could make for a good booster option for populations where BA.5 is surging.
Pre-print hoopla: COVID-associated neurodegeneration & Risks of subsequent infections
Two pre-prints generated a lot of attention recently.
Outcomes of SARS-CoV-2 Reinfection (Al-Aly, Bowe, Xie)
A large cohort study using US Dep. of Veterans Affairs data looked at the mortality and morbidity associations between first infections, re-infections and the non-infected.
This data found that re-infection was associated with further increases in mortality, hospitalisation and morbidity, regardless of vaccination status.
While this was erroneously reported as 'subsequent infections are worse' it appears more accurately to show that there is (likely) a cumulative health burden to reinfection with COVID. This should not surprise us. However we should temper our concern by noting that this says nothing about the 219,000 study participants (85%) who did not suffer a reinfection, or about those who were unknowingly reinfected, but for whatever reason were not tested.
Retrospective cohort studies like this, even when very large, are acutely sensitive to confounders. Arguably this study selected those with re-infections and symptoms, as these were the group most likely to present for care. Additionally 90% of subjects were men - so take it all with a pinch of salt.
Regardless, you should try hard to avoid any COVID infection, whether it is your first or your third. There is no COVID infection that it better than non-infection!
COVID and neurodegenerative risk (Zarifkar)
The second pre-print to get us all hot & bothered was Danish data presented by Zarifkar at the recent European Academy of Neurology (EAN) Congress.
Among over 35,000 COVID-positive patients there was an associated increased relative risk for Alzheimer's (RR, 3.5, 95% CI 2.2-5.5), Parkinson's (RR 2.6, 95% CI 1.7-4.0), ischaemic stroke (RR 2.7, 95% CI, 2.3-3.2), and intracerebral haemorrhage (RR 4.8, 95% CI 1.8-12.9).
Buuuuut, and here's the problem, for all of those morbid end-points (except ischaemic stroke) a similar association was seen for influenza infection or "after other common respiratory tract infections".
Clearly COVID (or Influenza) is not causing Alzheimer's disease (a progressive chronic disease usually occuring over decades), but it is feasible that a systemic inflammatory insult could hasten progression of existing neurodegeneration. There may also be confounding factors, such that the same comorbidities associated with neurodegeneration are also associated with infection, severe COVID illness, or simple seeking out a test.
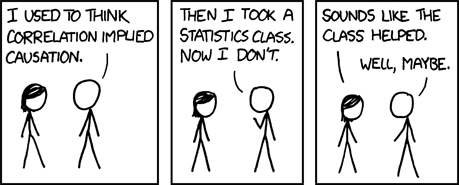
These large-population observational studies are clearly interesting, but we need to be careful to avoid rushing straight down the causation-highway. Remember that before falling in with the crazy COVID-minimiser crowd (🙄), legendary meta-researcher Dr John Ioannidis' published landmark research showing that 80% of conclusions from observational studies were later disproven.
Food for thought.
Some more COVID reading...
Despite the 39,000 COVID-related publications indexed by metajournal, it's easy to drill down into more relevant research and seperate the signal from the noise.
Click on Search... and then Reviews to narrow the COVID results to only the Latest COVID Review Articles.
Case in point, the latest edition of Critical Care Clinics has a big COVID focus, including reviews of COVID critical illness post-sequalae, COVID and acute kidney injury, the role of thrombus in COVID-19, Multisystem inflammatory syndrome in children, and COVID in the critically ill pregnant patient.
Of course, don't worry, plenty more COVID research still to come...


